Print — The Washington Post — Jan. 3, 2012
Study shows how virus distorts immune system
 Researchers at the National Institutes of Health call the 1918 influenza pandemic “the mother of all pandemics,” and with good reason: The flu virus infected around a third of the world’s population and killed at least 50 million people.
Researchers at the National Institutes of Health call the 1918 influenza pandemic “the mother of all pandemics,” and with good reason: The flu virus infected around a third of the world’s population and killed at least 50 million people.
Almost a century later, scientists have a better understanding of how most of those people died. They believe the culprit wasn’t influenza itself but immune system overreactions triggered by the virus.
And it wasn’t just in 1918. The 2009 swine flu killed more than 18,000 people worldwide, according to the World Health Organization. Scientists say immune overreactions caused the majority of those fatalities.
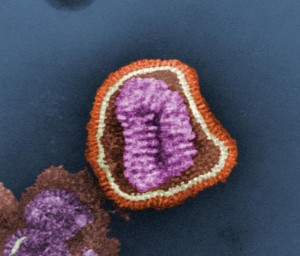
New research about how the virus works on the cellular level has uncovered what makes influenza so deadly: It destroys its host — you — by using your body’s own defenses against itself.
The research about such exaggerated immune responses could lead to more-effective flu drugs and radically change the way all kinds of infections are treated, leading virologists say.
“This is where the science [on epidemiology] is right now,” said Trish Perl, a senior epidemiologist at Johns Hopkins Hospital. “That’s what happens with a lot of severe infections. . . . It’s almost like the system goes into overdrive.”
While trying to destroy flu-infected cells, your immune system also destroys legions of perfectly healthy cells all over your body. This is why, even though the virus itself rarely ventures outside the lungs, the symptoms of the flu are so widespread, according to Michael Oldstone, a virologist at the Scripps Research Institute in La Jolla, Calif.
“If you get a cold or the flu, you get fever, pains, upset stomach,” Oldstone said. “That’s all due to the immune response.”
About this story
This story was written for the Health & Science section of The Washington Post. It is reproduced here as it was originally published on page E1 of the Post’s Jan. 3, 2012 edition.
Fatal attraction
Most of the time, this immune response isn’t too severe. As the virus runs its course, the response subsides. But in some cases, an infection can trigger a reaction so destructive it can be fatal. Scientists call this a cytokine storm, because of the violent way immune cells respond to a virus. (A cytokine is a molecule that immune cells use to send signals between one another.) Cytokines usually help fight off infections by telling the immune system which specific viral cells it should be attacking. But sometimes an overabundance of cytokines floods into a part of the body, and that’s when you get a storm.
Cytokine storms are rare, but Perl said they may be more common among younger people because they have stronger immune systems, which are more prone to overreactions. She said this may explain one of the more surprising outcomes of the 2009 swine flu: that it was deadlier among young people than it was among the elderly.
During flu infections, Oldstone said, cytokine storms can cause serious damage throughout the body, especially in the lungs. This, he said, combined with the lung damage cause by the influenza virus itself, leads to fatal cases of pneumonia.
Oldstone and two other researchers have been looking into cytokine storms for more than five years. They’ve identified a receptor on an endothelial cell called S1P1, and found that S1P1 signaling by endothelial cells initiates the cascade of events leading to a cytokine storm. The virologists’ findings, published in a recent issue of the scientific journal Cell, could pave the way for a new class of immune-reaction-blocking drugs that could be more effective than antiviral drugs.
“It is likely that a single oral dose of a compound can be developed that will provide protection against cytokine storms,” Hugh Rosen, Oldstone’s colleague at the Scripps Institute who also worked on the cytokine study, said in a statement.
The findings “could potentially change the way the flu is treated,” Oldstone said, and could even have implications for lung infections, HIV and other viral diseases, though Perl notes that the research on how cytokine storms function in these other diseases is still very unclear.
‘Getting under the hood’
Rosen, Oldstone and their team, with funding from the National Institutes of Health, examined this exaggerated immune response in mice.
The researchers injected one group of 30 mice with a strain of the H1N1 swine flu virus from 2009. Those mice were left untreated, and 80 percent of them died. The researchers injected 30 other mice with the virus, but they also gave this group an antiviral drug similar to Tami-
flu. Around half died.
For a third group of flu-infected mice, the researchers used an experimental cytokine-blocking compound instead of Tamiflu. Only 20 percent of these mice died.
And when the scientists gave a fourth group of mice both Tamiflu and the compound, the death rate dropped to 5 percent.
Cytokine-blocking drugs could be more effective than antivirals, Oldstone said, because they target the flu effects that cause the most damage to the body. Also, a problem with many antiviral drugs is that they can cause viruses to mutate into drug-resistant strains. Oldstone said that probably wouldn’t be an issue for cytokine-blockers because they don’t affect the virus itself.
Jeff Dimond, a spokesman for the Centers for Disease Control and Prevention, said Oldstone and his colleagues went deep into the cellular level to figure out how cytokine storms function. “This is really ‘getting under the hood and tinkering with the wires’ research,” he said.
Dimond said CDC scientists are also looking at links between the immune system and flu fatalities.
Oldstone said there’s still much that scientists don’t understand about cytokine storms. For example, he said, it’s unclear why the flu virus causes a life-threatening storm in some people while for others it produces nothing more than a few miserable days at home.
While Oldstone’s findings may lead to better flu-fighting drugs, it will probably be many years before those drugs reach the local pharmacy. He said the next step for his team is to try to replicate the mouse study using ferrets, then primates and then, finally, humans.
In the meantime, Perl said, scientists now know much more about how the immune system functions and, more important, how it malfunctions. “It’s even more complicated than what we were taught in med school,” she said.